
1-7 November 2017
Join us for fertility discussions, advice & support
Despite the substantial evidence of age-related decline in fertility, many people are unaware of the risks associated with delaying childbearing.
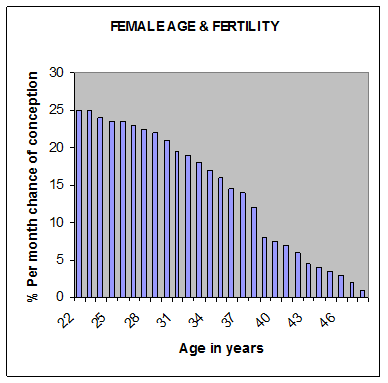
In most women, fertility is highest until about 30 years of age and then declines, with especially sharp declines from 35 years. Male fertility probably declines from around 50 years. As more people choose to delay childbearing, increasing numbers will face age-related fertility problems. A study of New Zealand university students (3) has revealed that New Zealand students have unrealistic beliefs about both the impact of age on fertility and success rates of fertility treatment. Most respondents (81%) indicated they wished to have children in the future, but planned to do this ‘late’ or ‘very late’. The students believed fertility treatment to be more successful than actual success rates. They also predicted fertility declined with age much later than it occurs in reality.
Women over 35 years of age are nearly twice as likely to present with unexplained infertility. The incidence of genetic abnormalities and spontaneous abortion also increases with age. For older people, it is very helpful to undergo a preconception health programme prior to conceiving to enhance their chances of a healthy pregnancy and child.
Plan your last child, not your first!
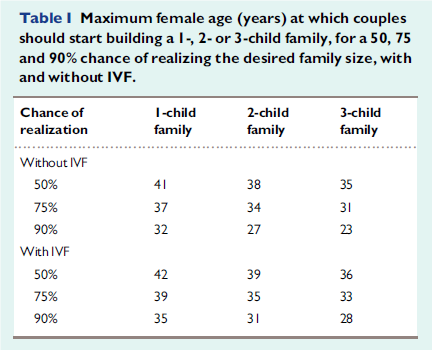
Couples and singles wishing to have children in the future should consider the number of children they want, together with the estimated chance of conception at various ages, particularly for the ‘last’ desired child.
Recently published data (2) illustrates the chance of having one, two or three children starting at various ages, with and without recourse to IVF (if needed).
When to seek help
Women – seek help straight away for any of the following:
- irregular cycles (short or long)
- getting periods less than 10 days after ovulation occurs
- severe pain with menstruation or intermittent pain throughout the cycle
- regular breakthrough bleeding throughout cycle
- any unusual discharge (yellow/green, lumpy white, smelly)
- previous sexually transmitted infections, such as Chlamydia
- a history of early menopause (before age 50) in the family
Men – seek help straight away for any of the following:
- previous genital surgery, including for an undescended testicle
- previous inguinal hernia repair
- previous significant infections such as Chlamydia or Mumps Orchitis
For a couple:
- When you have been trying to conceive for longer than 12 months. You can see your GP first who may be able to refer you for a funded consultation or you can book a private appointment directly with a fertility specialist. The first step is likely to include blood tests to check ovulation and a semen analysis, which your GP can conduct.
- If the woman is over 35 years, see your doctor after trying to conceive for 9 months
- If the woman is over 40 years, see your doctor after trying to conceive for 6 months
Your GP can organise further testing and may be able to refer you for a funded consultation with a fertility specialist.
Making Babies DIY Webinars
Join us here for this free-of-charge webinar. There will be presentation live on screen, followed by Q&A. Bring your questions, ready to type into the box! View the full Webinar schedule here
Know your mother’s age at menopause and/or have an AMH test
Mother’s age at menopause can help improve the prediction of your likely age at menopause. If your mother was younger than 50 at menopause, you may be advised to take an AMH test or consider trying to conceive earlier. Note that egg quality declines significantly in the 10–20 years prior to menopause – menstruation does not mean that you are likely to become pregnant. Fertility virtually stops 5–7 years before menopause – there is only a very low chance of natural conception.
An AMH test is a measure of your ovarian reserve (how many eggs you have left). Although it is not a precise predictor of when you will reach menopause, or how likely you are to conceive, it gives an indication of your ovarian reserve compared with the average woman of the same age. AMH results should be considered in conjunction with other factors, including time of trying to conceive, fertile mucus and FSH results.
Age effects on men’s fertility
A man’s age is also significantly related to fertility problems. Overall, male age is associated with a decline in semen volume, sperm motility, and sperm morphology. After accounting for female age, comparisons between men under 30 and men over 50 years found relative decreases in pregnancy rates of 23–38% (1).
Sperm motility and the number of healthy sperm might decline after 50 years of age, affecting a man's fertility. Some research suggests that women who become pregnant by older men have a slightly higher risk of miscarriage. A father's increasing age has also been associated with a higher risk of autism, schizophrenia and new (not inherited) genetic abnormalities in children.